www.apjph.comwww.apjph.com

Ref Number = ASPR0014
Infectious Disease: Old problems, New Challenges
Anggraini Alam Infection and Tropical Diseases Working Group Indonesian Pediatric Society Dept. of Child Health Universitas Padjadjaran/Hasan Sadikin Hospital
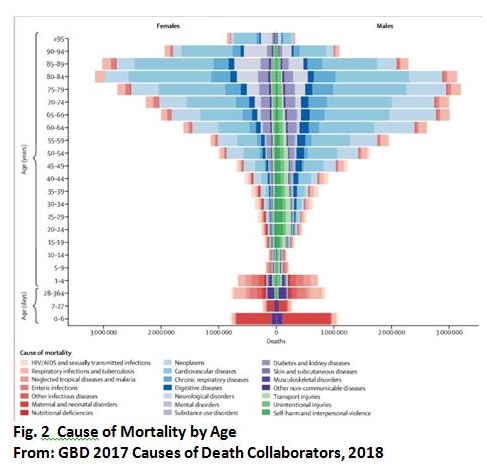
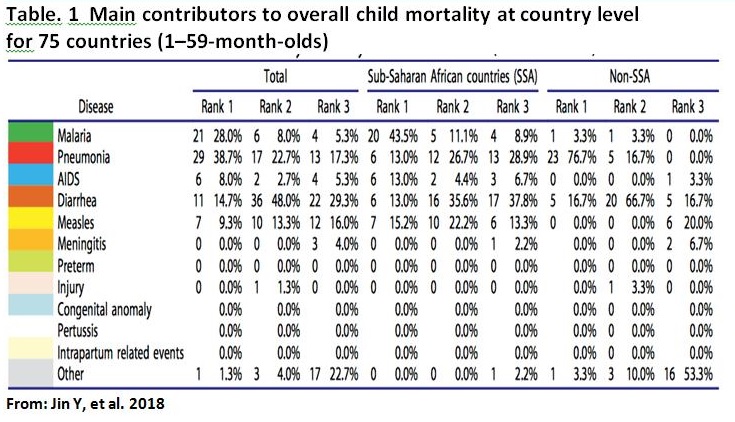
Introduction In this globalized world, the human species is endangered by infectious diseases. We face newly emerging threats, such as, new influenza virus variants, new pathogenic microbes, especially those transmitted from animals, resurgent infections such as TB, resistance to antimicrobial drugs and the threat of bioterrorism. Only two diseases, smallpox and rinderpest, have been eradicated. Our planet is a potential ?hot spot? for emerging and re-emerging infectious diseases??. The scope of International Health Regulation (IHR) and the timing of its introduction, were influenced by the emergence in China of the coronavirus that caused severe acute respiratory syndrome (SARS) in 2003. It is now mandatory to report to WHO any case of SARS, plus smallpox, polio, and any new viral subtype of human influenza. According to IHR, WHO must also be notified of other infections that may constitute public health emergencies of international concern, following an assessment of their public health impact. These include, but are not limited to, cholera, pneumonic plague, yellow fever and viral haemorrhagic fevers, including Ebola, Marburg and Lassa. However, the scope of the new regulations is wider and includes events other than infections, such as chemical spills and nuclear accidents (figure 1). ASPR0014 - 1 We are the witnesses and also the pilots and victims of a new, disrupted system, where the old rules of limited mutual interaction are no longer valid. Frontiers are abolished; free circulation of man and products is the rule; human immigration into cities leads to new microbial concentrations; massive influence of civilization on the environment reshuffles epidemiologic conditions ? infectious diseases in particular and health in general have also become globalized The Epidemiological Transition The epidemiological transition, interlinked with the demographic transition, provides the central narrative of global health. The transition begins with a fall in the death rate, mainly from acute infectious diseases of childhood. Through time, infectious diseases of childhood are replaced by the chronic, non-infectious diseases typical of adulthood in larger, older populations. The majority of these deaths have been and will be caused by just a few pathogens. Among the 1400 or so recognized human pathogens and parasites, two-thirds of deaths from infections in 2010 were caused by around 20 species, mainly bacteria and viruses, but, these statistics on infectious diseases, which count deaths mostly from endemic infections, exclude the threat of epidemics and pandemics. Among all infectious pathogens, bacteria represent the principal cause of death in young children, accounting for more than a third of all child deaths globally. The etiology is largely due to vaccine-preventable infections. Despite the availability and application of clinical procedures for microbiological diagnosis, the causative organism remained unidentified in approximately 50% of patients. Patients in whom a causative organism was identified seemed to have had a more severe disease than those in whom the cause of infection was unknown: the length of hospital stay was longer, and a higher proportion of patients required PICU admission, respiratory support, and supplemental oxygen. For infectious diseases, whether exposure to a pathogen leads to the establishment of infection and to illness, and the outcome of a course of illness depend on the nature of the pathogen and associated risk factors. The most victims of infectious diseases are young children. Infectious illness was ?the single largest cause of death in children dying of an acute physical illness? worldwide in 2013, constituting ?20% of the deaths overall?, and with children aged 1?4 years being the most affected. Among all infectious pathogens, bacteria represent the principal cause of death in young children, accounting for more than a third of all child deaths globally (Figure 2). ASPR0014 - 2 Wide disparities existed across causes within countries, both in neonatal and post- neonatal mortality reduction. In 20 of the 45 sub-Saharan African countries, malaria was the main contributor to post-neonatal mortality reduction, and pneumonia was the main contributor in only six countries. A single disease often contributed to a substantial proportion of the child mortality reduction, particularly in West and Central African countries. So, the child mortality had country-specific characteristics with regards to cause-wise child mortality that could not be identified by global analyses. A study showed main contributors to child mortality which separate between Sub-Saharan African and other countries outside Africa (Table. 1). ASPR0014 - 3 Why Children Are Especially Vulnerable Children are particularly vulnerable to rapid spread of infectious diseases and exposure to toxic substances for several reasons. Young children, especially infants and toddlers, have a natural curiosity that leads to frequent and wide-ranging handling of objects and surfaces and a tendency to put their hands and objects in their mouths without concern about washing first. Since their immune systems are still develop- ing, and because children are smaller than adults, they often have a more pronounced reaction to infections and other sub- stances. Sometimes, this is referred to as a higher physiologic dose/effect per unit exposure. Children are highly vulnerable to aerosolized biological or chemical agents because they normally breathe more times per minute than adults. As a result, they receive larger doses in the same period of time. Also, because such agents are heavier than air, they accumulate close to the ground, in the breathing zone of children. Children are more vulnerable to agents that act on or through the skin because their skin?is thinner and they have a larger skin surface-to-body mass ratio than adults. Children are more vulnerable to the effects of biological and chemical agents that produce vomiting or diarrhea because they have smaller body fluid reserves than adults, increasing the risk of rapid progression to dehydration or shock. Most importantly, children are dependent on others for their care (eg, they would not be especially good about rehydrating themselves without guidance). For these and other reasons, children need direct supervision (by sight and sound) especially during and after an outbreak or emergency situation. Types of Infectious Disease Emergencies When a strange type of illness occurs, or an unusual number of individuals develop an illness or symptom, the situation may be an outbreak, an epidemic, another type of infectious disease emergency, an environmental issue, or an incident of bioterrorism. An outbreak is a sudden rise in the occurrence (the number of cases) of a disease. Some outbreaks are expected?each year, like influenza, hand-foot-and-mouth disease, and bronchiolitis. Other outbreaks need to be reported to the public health authorities, especially those where public health officials can advise about control measures and help ensure accurate communications among health professionals, child care personnel, and parents. An outbreak of an unusual or severe illness must be reported to public health authorities immediately. An epidemic is the occurrence of more cases of disease than would be expected in a community or region during a given period. The term is similar to an outbreak, but it usually is used to describe an unusual frequency of illness in a group of people that is not explained by the usual seasonal increases. The term outbreak might be used when a single case of an unusual disease occurs. A pandemic is an epidemic that spreads through human populations worldwide. Because there have been previous situations where a pandemic influenza has happened, public health officials are engaged in ongoing efforts to prepare for this type of a situation. The term bioterrorism is used to describe a situation in which a biological agent is intentionally released to cause illness. The biological agent involved in bioterrorism may be?a living germ or a poison, such as anthrax, ricin, or botulism toxin. If a group of children and adults become ill with similar symptoms at the same time, the public health authorities should be notified. They will consider bioterrorism as one of the possibilities as well as the more likely event of an out- break of common infectious disease. Public health officials are likely to be more sensitive to such reports if there are signs of certain rare infections (like anthrax or smallpox) that are unusual as ?natural? occurrences. The list of new organisms or re-emergent organisms is, by definition, incomplete, constantly changing and operational. Figure 3 illustrates some examples of emerging and reemerging infections throughout the world in recent years. Some, such as Ebola virus and Nipah virus, have been highly virulent but have involved relatively small numbers of people, have remained tightly restricted in their spread, and so have been more medical curiosities than global public health threats. Figure 3 is not intended to give a complete overview, but rather to show the immense diversity of the most important emergent pathogens. Such a list would not be complete without mentioning another type of emergent epidemic, maybe the most important one, also caused by our own mismanagement ? the new epidemic of multidrug resistance. Multidrug-resistant malaria, have involved large numbers of people but have, because of the demography of the infection, remained for the most part geographically restricted. This has resulted in a serious situation in the region involved but not a global public health threat. Multidrug-resistant tuberculosis and vancomycin-resistant Staphylococcus aureus and enterococci are examples of emerging infections that do not immediately involve large numbers of persons but that will ultimately have a serious impact on public health throughout the world. ASPR0014 - 4 The discovery and development of antimicrobials, only 60 years ago, has indeed added a formidable pressure on the microbial population in contact with the human species. However microbial adaptation has been not only multifaceted, but also fast when compared to the previous evolution of life. So far, resistance to antimicrobials has developed among any pathogen (bacteria, viruses, parasites) exposed to any new antiinfective agents. The growing problem of antibiotic resistance carbapenems are the major last-line class of antibiotics to treat infections with multidrug-resistant (MDR) Gram-negative bacteria such as Klebsiella pneumoniae (a frequent cause of pneumonia and urinary tract infections in hospitals). These 15?50% of K. pneumoniae from bloodstream infections are resistant to carbapenems in Western countries. Staphylococcus aureus, a bacterium that can cause a variety of infections (from minor skin infections to severe pneumonia). Its adaptation has led to an MDR pathogen, methicillin-resistant S. aureus (MRSA). MRSA is associated with severe invasive disease. Initially, MRSA was only a nosocomial pathogen, but in the last 20 years it has been identified in the community (community-associated (CA)-MRSA). The frequency of CA-MRSA pneumonia can be estimated to be between one in 200 and one in 2,000 cases of CAP. CA-MRSA pneumonia is a severe disease with 75?85% of affected patients being admitted to the intensive care unit and 20?60% dying. Although there is no immediate public threat, mcr-1 brings to the forefront the global challenges in addressing antibiotic resistance and best practices for antibiotic use. The mcr-1 gene causes resistance to colistin, which is considered by the CDC to be a ?last resort antibiotic?. The Role of Infectious Diseases Doctor and The Organization Infectious diseases in modern times can only be comprehended as a science with a new approach acknowledging the environment as one of the important players in the field; hospital and public health, geographical, societal and political strategies have to be included in eradication strategies. The modern infectious diseases specialist has therefore to be a socially conscious, responsible person; collaboration with other specialist and subspecialist, and the most important is The Pediatric Society ? per se the Pediatricians should encourage the stake holder to perform political will of reduction the infectious diseases problems in community. Areas of general interest and importance, and in which rapid progress should be made include the following: ? Sustainability, in order to prevent the irreversible transgression of critical thresholds (ocean belt conveyors, ice shield, ozone layer, rain forests) which could alter dramatically our living conditions ? ? Epidemiology, with an expansion into new fields driving this science, such as economic, social, behavioural contexts ? ? Collective action: setting up and implementing general rules and regulations for migrants, refugees, travel, antibiotic misuse, food market and network; in addition, all these changing conditions require the development of a vast early global warming system, needed high performance computer networks ? the grids ? set up by physicists and mathematicians ? ? Public health practices have to be rapidly and dramatically improved and collective action at the population level is rapidly required. In particular, the problem of water access should be put on national and international agendas and prioritized within the next few years, if we want to avoid a major political crisis or a mere economic solution to the problem ? ? Control of the human and non-human usage of anti-infectives will become a necessity, and it is high time to reinforce the established rules and regulations, if we do not want the era of antibiotics to come to a rapid end. ? So far, we have relied mostly on conventional methods, logistics and tools, but new domains in science are developing rapidly which we may take the advantage. Challenges in The Eradication of Infectious Diseases In order to be successful, eradication effort has to permanently eliminate a pathogen everywhere in the world. Pathogen prevalence is globally, hopefully, reduced to zero, thereby removing the risk of re-introduction and re-establishment. Elimination, on the other hand, is a more localized effort that focuses on reduction to zero incidence of a certain pathogen in a given area, with active measures to prevent pathogen re-establishment from other areas after elimination. Since eradication is elimination on global scale, there are many similarities between those two efforts, particularly in dynamical transitions from endemic transmission to elimination and post-elimination period of enhanced vigilance. Once infection is driven to very low levels, the ecology of pathogens may change requiring different surveillance and control strategies. The dynamics of infectious diseases close to elimination can be distinctly different from natural dynamics. The distribution of susceptibility is no longer governed by a combination of replenishment of the susceptible population through births, and immunity through past exposure but, instead, by vaccination coverage, the extent of mass drug administrations (in the case of many campaigns against neglected-transmitted diseases/NTDs or behavioural changes (e.g. guinea worm that is on track to be eliminated without the use of drug or vaccine. New opportunities and strategies This expanding new universe of inter-bacterial communication offers totally new avenues for useful applications in biotechnology, ecology, and human diseases. Substances inhibiting cell-to-cell communication could well avoid the establishment of bacterial invasion and represent a new generation of antimicrobials which are less prone to the emergence of resistance. By 2001, 37 microbial genome sequences had been completed, and 142 were in progress worldwide. The recent development of robotics to achieve high spotting densities of DNA, allows the construction of microarrays containing up to 50,000 genes on a single microscopic slide. This sequencing technique helps to accumulate important data that could usefully answer many important questions regarding human pathogens, such as bacterial evolution, identification of potential virulence genes, analysis of epidemics and rapid diagnostic methods in clinical microbiology. Nanotechnology and nanobiology In recent years, remarkable progress has been achieved at an ever lower level of the life scale ? at the level of the nanometer. Search for drug discovery and delivery is moving smaller drug targeting against tumour vessels for instance has become now a reality, and many new biologically active nanostructures are being developed: ?Macrodoctors, come meet the nanodoctors? is soon to become a reality. Vaccinology Modern vaccinology has also made spectacular progress in recent years by the use of the most modern technologies. The list regarding the production of active immunization systems is indeed impressive. The eradication of many diseases around the world has now become a realistic goal. Long term consequences of chronic diseases, such as hepatitis B-induced hepatoma, have been clearly shown to be drastically reduced. New vaccine strategies are being explored, such as the use of conjugated vaccines, recombinant proteins, pseudovirions and DNA vaccines. Delivery systems are also improving with the exploration and implementation of transdermal applications, microencapsulation and plant expression of antigens. It is hoped that research in this field will soon help to control, at affordable prices, diseases such as malaria, HIV, and M. tuberculosis. A Identify Post-Eradication Opportunities and Threats Finally, in the event of successful elimination/eradication how long do we need to hold the line? Should one invest in maintaining herd immunity, or implement low-level indefinite control, or stop with the efforts altogether (as with smallpox)? If we were to scale down or stop control efforts, when would it be safe to do so? Should we switch to a different strategy and, if so, when? What are the spatial strategies for maintaining freedom from disease? What defines the width of a protective sanitair and how should elimination efforts be coordinated across international boundaries? Detection of low-level infection requires ever more sensitive and more accurate detection methods, so surveillance abilities are crucial in post-eradication strategies. Measuring loss of herd immunity or finding asymptomatic carriers might require new surveillance and monitoring techniques and better statistical tools in analysis of the relevant data. All of these need to be considered in a dynamical framework to predict possible shifts in dynamical regimes or potential tipping points for re-emergence of eliminated pathogens or emergence of related ones through competitive release in vacated niches. Eradication initiatives require sustained public health, political, financial and individual efforts. It is a dynamical challenge that requires vast data integration over temporal, geographical and socioeconomic scales. As always ? the long itinerary of research from the bench to the bedside. Yet the inherently dynamic nature of infectious diseases can also have unexpected advantages. Models demonstrated malaria elimination to be a surprisingly stable state, indicating that elimination could be incrementally achieved without needing the simultaneous and correspondingly expensive effort as required for say polio. The eradication endgame poses a diverse set of challenges that can be addressed in a modelling framework leading to improved surveillance and control. Conclusions The under-5 mortality rate were still high with cause of dead are infectious diseases. In contrast to other human diseases, infectious diseases may be unpredictable with the potential for global outbreaks. the epidemiological transition provides the central narrative of global health. Critical to our ability to meet the challenges of infectious diseases in the 21st century is the continual and rapid evolution of the scientific and technological advances that serve as the foundation for the response of the public health. The pediatrician needs to encourage the stake holder in performing political will of reduction the infectious diseases problems.


Refference:
Dye C. 2014 After 2015: infectious diseases in a new era of health and development. Phil. Trans. R. Soc. B 369: 20130426. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018; 392: 1736-88. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990?2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018; 392: 1789?858 Irwin AD, Drew RJ, Marshall P, et al. Etiology of childhood bacteremia and timely antibiotics administration in the emergency department. Pediatrics. 2015; 135: 635?42.? Jin Y, Mankadi PM, Rigotti JI, Cha S. Cause-specific child mortality performance and contributions to all-cause child mortality, and number of child lives saved during the Millennium Development Goals era: a country-level analysis. Global Health Action. ?2018; 11: 1546095. Klepac P, Funk S, Hollingsworth TD, Metcalf CJE, Hampson K. Epidemics. 2015; 10: 97?101. Liu L, Oza S, Hogan D. Global, regional, and national causes of child mortality in 2000?13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet 2015; 385: 430?40. Martin NG, Sadarangani M, Pollard AJ, Goldacre MJ.?Hospital admission rates for meningitis and septicaemia caused by Haemophilus influenzae, Neisseria meningitidis, and Streptococcus pneumoniae in children in England over five decades:?a population-based observational study. Lancet Infect Dis. 2014; 14: 397?405.? Pearson GA, Ward-Platt M, Kelly D. How children die: classifying child deaths. Arch Dis Child. 2011; 96: 922?26. Pen ?a AE, Ostfeld RS, Peterson AT, Poulin R, Fuente J. Trends in Parasitology. 2014; 30(4). Saronson SS, Shope TR. Managing Infectious Diseases in Child Care and Schools, 4th Ed. ebooks.aappublications.org/managing-infectious-diseases-in-child. Torres FM, Salas A, Calle IR, L
Disclaimer: The Views and opinions expressed in the articles are of the authors and not of the journal.
Editor-In-Chief
Journal Office
Mid City Hospital, 3-A Shadman II
Jail Road, Lahore ,Pakistan
Mid City Hospital, 3-A Shadman II
Jail Road, Lahore ,Pakistan
Managing Editor
Dr. Intan Juliana Abd Hamid
Support & Help
Support & Help
Assistant Editor
Dr. Sadia Shabbir Hussain
Support & Help
Support & Help
Digital Content Editor
Dr. Khalid Masud
Administrator
Administrator