www.apjph.comwww.apjph.com

Ref Number = ASPR0016
Cholestatic Children: From Vitamin D Insufficiency to Osteoporosis
Bagus Setyoboedi Department of Child Health University of Airlangga/Dr. Soetomo Academic General Hospital, Surabaya, Indonesia E-mail: baguzze@gmail.com
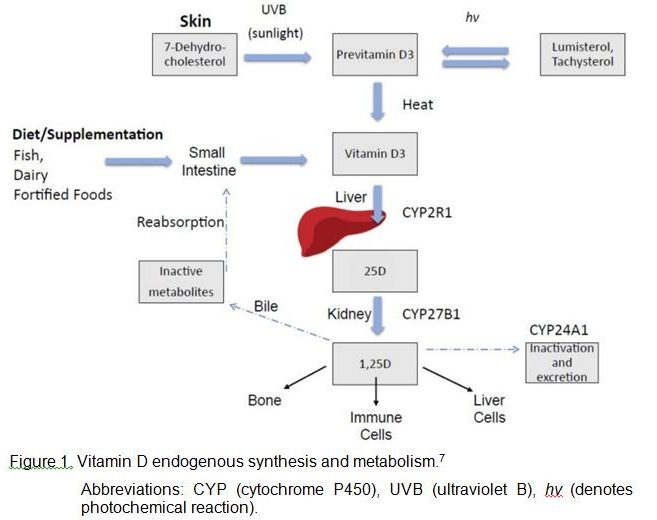
Patients with cholestatic liver disease are particularly susceptible to osteoporosis due to the interference of cholestasis with vitamin D metabolism.1 Osteopenia and pathologic fractures have been reported in children with chronic cholestatic liver disease, including Alagille syndrome (ALGS), progressive familial intrahepatic cholestasis (PFIC), and biliary atresia.2,3,4 Cholestasis is a pathologic state of bile reduction or abnormal flow into bile ducts resulting in an elevated conjugated serum bilirubin and bile salts concentrations consequently mal-absorption of vitamin D takes place especially those unexposed to the sun due to their chronic illness. 5 Children who had a higher serum bilirubin level were more likely to be vitamin D-deficient and may benefit from a much higher vitamin D supplement or parenteral route.6 Endogenous vitamin D synthesis occurs primarily through sunlight exposure which produces pre-vitamin D3. It is hydroxylated in the liver and then in the kidney, producing 1,25D (1,25 dihyroxyvitamin D), the physiologically active form of vitamin D which acts in target sites in bone and immune cells, as well as liver cells (Figure 1).7 Vitamin D3 is hydroxylated in the liver to 25-hydroxy vitamin D (25-OH-vitamin D) and then in the kidneys to 1,25-hydroxyvitamin D Decreased 25-OH-vitamin D production is associated with altered liver function and it results in impaired osteoclast-mediated bone resorption, osteoblast-mediated mineralization and decreased calcium resorption in the gastrointestinal tract. Additionally, disturbed secretion of bile leads to decreased fat absorption and abnormal uptake of vitamin D as a result. To summarize, disturbed metabolism of calcium and vitamin D results from impaired 25-hydroxylation, intestinal malabsorption and decreased skin synthesis in patients with jaundice.8 ASPR0016-1 Osteoporosis is a disorder of low bone mass, microarchitectural malformation and structural weakness while osteomalacia is a disorder of decreased osteoid mineralization at sites of bone formation. The etiology of bone loss is multifactorial and not entirely understood. Patients with cholestatic liver disease are particularly susceptible to osteoporosis due to the interference of cholestasis with vitamin D metabolism.1 Clinical conditions for which early diagnosis of osteoporosis are indicated are given in Table 1.9,10 ASPR0016-2 The pathogenesis of bone loss in liver patients is poorly understood.10 Reduced bone density in children with cholestatic liver disease is multifactorial and related to growth, degree of cholestasis, fracture vulnerability, and contribution of underlying genetic etiology.11 The pathogenesis of osteoporosis in chronic liver disease is complex and related to both increased bone resorption12 and reduced bone formation9. Unstable bone remodeling is caused by a number of mechanisms, some of which remain unknown. In many cases, the mechanisms of impaired bone metabolism are largely caused by the unique characteristics of the specific liver disease being considered. However, there remain a number of common factors related to chronic liver disease in general that affect bone metabolism. These include vitamin D and calcium metabolism alterations, vitamin K deficiency, and hormonal dysregulation, the release of cytokines and deficiency of insulin-like growth factor 1 (IGF-1).1 The management of bone disease in liver patients is addressed to reduce or avoid the risk factors for osteoporosis and fracture. For the prevention and treatment of osteoporosis good nutrition is recommended, as are the suppression of the risk factors for osteoporosis and the administration of supplements of calcium and vitamin D. There is no specific treatment for osteoporosis, although it has been demonstrated that bisphosphonates, especially weekly alendronate and monthly ibandronate, are effective in increasing bone mass in patients with chronic cholestasis.10 In contrast to what is seen in adults, children have remarkable improvement in bone mineral density (BMD) by 1 year after liver transplantation, often accompanied by significant catch-up growth.13
Keywords: cholestasis; children; vitamin D; osteoporosis

Refference:
1. Handzlik-Orlik G, Holecki M, Wilczy?ski K, Du?awa J. Osteoporosis in liver disease: pathogenesis and management. Ther Adv Endocrinol Metab. 2016 Jun;7(3):128-35. 2. Bales CB, Kamath BM, Munoz PS, Nguyen A, Piccoli DA, Spinner NB, et al. Pathologic lower extremity fractures in children with Alagille syndrome. J Pediatr Gastroenterol Nutr. 2010;51:66-70. 3. Chen HL, Chang MH. Growth failure and metabolic bone disease in progressive familial intrahepatic cholestasis. J Pediatr Gastroenterol Nutr. 2004;39:328-330. 4. Chongsrisawat V, Ruttanamongkol P, Chaiwatanarat T, Chandrakamol B, Poovorawan Y. Bone density and 25-hydroxy vitamin D in extrahepatic biliary atresia. Pediatr Surg Int. 2001;17:604-8. 5. Anwar MM, Arafa AE, Morgan DS, Mohamed KK. Association between vitamin D level and patients with cholestasis. Int J Community Med Public Health. 2018 May;5(5):1713-17. 6. Lee WS, Jalaludin MY, Wong SY, Ong SY, Foo HW, Ng RT. Vitamin D non-sufficiency is prevalent in children with chronic liver disease in a tropical country. Pediatr Neonatol. 2019;60(1):12-8. 7. Keane JT, Elangovan H, Stokes RA, Gunton JE. Vitamin D and the liver-correlation or cause? Nutrients. 2018 Apr 16;10(4). pii: E496. 8. Van Leeuwen J, van Driel M, van den Bemd G, Pols H. Vitamin D control of osteoblast function and bone extracellular matrix mineralization. Crit Rev Eukaryot Gene Expr. 2001;11: 199?226. 9. Collier, J, Ninkovic, M, Compston, J. Guidelines on the management of osteoporosis associated with chronic liver disease. Gut. 2002;50(Suppl.1): 1?9. 10. Gua
Disclaimer: The Views and opinions expressed in the articles are of the authors and not of the journal.
Editor-In-Chief
Journal Office
Mid City Hospital, 3-A Shadman II
Jail Road, Lahore ,Pakistan
Mid City Hospital, 3-A Shadman II
Jail Road, Lahore ,Pakistan
Managing Editor
Dr. Intan Juliana Abd Hamid
Support & Help
Support & Help
Assistant Editor
Dr. Sadia Shabbir Hussain
Support & Help
Support & Help
Digital Content Editor
Dr. Khalid Masud
Administrator
Administrator