www.apjph.comwww.apjph.com

Ref Number = ASPR0023
Cardiovascular Complication in Children with Anemia
Erling David Kaunang, MD, PhD, Pediatric Consultant a* a Department of Pediatrics, Faculty of Medicine, Sam Ratulangi University, Manado, Indonesia *E-mail: drdavidkaunang@yahoo.com
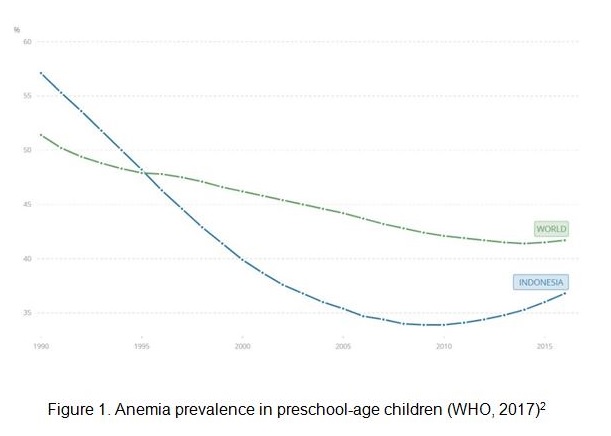
Anemia is not a specific disease entity but is a condition caused by various underlying pathologic processes, which may be acute or chronic.1 Globally, anemia affects around 1.62 billion people, which corresponds to 24.8% of the population, with highest prevalence in preschool-age children (41.7%).2 In Indonesia, Basic Health Research (Riskesdas) in 2013 reported child anemia prevalence of 28.1% (age 1-5 years) and 26.4% (age 5-14 years).3 WHO in 2017 reported Indonesia?s anemia prevalence in preschool-age children of 36.8% (see figure 1).2 Anemias are classified based upon red blood cell (RBC) size and the physiologic response of the bone marrow / reticulocyte response. Approaching the evaluation of an anemic patient using these classification schemes helps to further narrow the diagnostic possibilities.4 ASPR0023 - 1 The main physiologic role of red blood cells is to deliver oxygen to the tissues. Certain physiologic adjustments can occur in an individual with anemia to compensate for the lack of oxygen delivery. These include (1) increased cardiac output; (2) shunting of blood to vital organs; (3) increased 2,3-diphosphoglycerate (DPG) in the RBC; and (4) increased erythropoietin to stimulate RBC production. These compensatory changes, however, require an increase in myocardial work and oxygen consumption at a time when myocardial oxygen delivery is decreased. These conditions subsequently resulted in myocardial ischemia.5 Cardiovascular compensatory consequences of anemia include tachycardia, increased cardiac output, hyperdynamic state due to reduced blood viscosity, and vasodilation to improve tissue perfusion. Anemia increases cardiac output, may lead to eccentric left ventricular hypertrophy, activation of the sympathetic nervous system, stimulation of the renin angiotensin aldosterone system, and is closely associated with chronic inflammation and increased oxidative stress.6 Cardiovascular complications of anemia are due to worsening of the hyperdynamic state, volume overload, cardiac dilation, valvular failure, and heart failure with increased cardiac output. Resting cardiac output increases only when hemoglobin concentration declines to 10?g/dL or less.7 Clinical cardiovascular manifestation in children with anemia includes: - Blood pressure abnormality Recognizing blood pressure (BP) abnormalities in children is more cumbersome than in adults, as each child has his/her own BP thresholds based on gender, age, and height percentile.8 In acute and severe case of anemia, compensatory mechanisms are no longer sufficient to maintain blood pressure, and clinical signs include postural hypotension, altered mental status, cool and/or clammy skin, tachycardia, and hyperventilation might occur.9 - Electrocardiography (ECG) changes Most common form of ECG alteration in children with anemia is tachycardia, which occurred as a physiological compensatory mechanism response. Other several electrocardiographic changes including ST segment depression, T wave inversion, QT interval prolongation, and reduced amplitude of the QRS complex.10 Anisocytosis, an early sign of anemia, and macrocytosis are also linked to prolonged QT intervals in hypertensive patients.11 - Heart failure. Congestive heart failure is uncommon in patients with anemia without underlying heart disease and may occur only in cases of severe anemia with hemoglobin of 5?g/dL or less.7 Anemia is a common comorbidity in patients with chronic heart failure and is associated with cardiovascular mortality, reduced oxygen carrying and storage capacity, impaired quality of life, and higher risk for hospitalization.12 Vitamin B12, folic acid, and iron deficiency may also cause / worsen anemia in heart failure patients.13 Some cases of anemia in childhood have hereditary causes that are well explained nowadays, such as thalassemia, sickle cell anemia, hereditary spherocytosis, hereditary pernicious anemia, Fanconi anemia, and thrombocytic thrombocytopenia purpura (TTP). The main cardiovascular effects of sickle cell disease and thalassemia are due to hypoxia and iron accumulation, respectively. Thromboembolic risk and lipid profile should be monitored after splenectomy in children with hereditary spherocytosis.14 Anemia is an important risk factor for morbidity and mortality in patients with congenital heart disease (CHD).15 Prevalence of iron deficiency anemia in CHD patients ranging from 9.0-13%.16-18 Another important comorbid factor of anemia in children with CHD is malnutrition. Prevalence of malnutrition in pediatric CHD patients is worryingly high, with reports ranging from 51% in Oman, to 55.9% in India.19,20 Correcting anemia in CHD patients is not a simple task, as there are many causes contributed to this condition. Therefore, early corrective intervention in CHD patients should be performed whenever indicated, to prevent further complexion in morbidity.16
Keywords: Pediatric Anemia; Cardiovascular Complication
Refference:
1. Badireddy M, Baradhi KM. Chronic Anemia. [cited 2019 Jul 21]. Treasure Island (FL): StatPearls Publishing; 2019 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534803/ 2. World Health Organization. Prevalence of anemia among children (% of children under 5) [cited 2019 Jul 21]. The World Bank Group. Available from: https://data.worldbank.org/indicator/SH.ANM.CHLD.ZS 3. Riset Kesehatan Dasar: Proporsi anemia penduduk umur > 1 tahun menurut karakteristik. Badan Litbang Kementerian Kesehatan Republik Indonesia, 2013. p256. 4. Brugnara C, Oski FA, Nathan DG. Diagnostic approach to the anemic patient. In: Nathan and Oski's Hematology and Oncology of Infancy and Childhood, 8th ed, Orkin SH, Fisher DE, Look T, Lux SE, Ginsburg D, Nathan DG, et AL (Eds), WB Saunders, Philadelphia, 2015. p.293. 5. Inoue S et al. Pediatric Acute Anemia [cited 2019 Jul 21]. Medscape Pediatrics: General Medicine, 2017. Available from: https://emedicine.medscape.com/article/954506-overview 6. Aronow WS. Cardiac Arrhythmias Mechanisms, Pathophysiology, and Treatment, In Tech, Rijeka, Croatia, 2014. 7. Metivier F, Marchais SJ, Guerin AP, Pannier B, and London GM. Pathophysiology of anaemia: focus on the heart and bloodvessels, Nephrology Dialysis Transplantation. 2000; 15(3): 14-18. 8. Bijlsma MW, Blufpand HN, Kaspers GJ, Bokenkamp A. Why pediatricians fail to diagnose hypertension: a multicenter survey. J Pediatr. 2014; 164(1): 173-7. 9. Alder L, Tambe A. Acute Anemia. [cited 2019 Jul 21]. Treasure Island (FL): StatPearls Publishing; 2019 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537232/ 10. Mozos I, Serban C, and Mihaescu R. Anemia and the QT interval in hypertensive patients. International Journal of Collaborative Research on Internal Medicine & Public Health. 2012; 4(12): 2084-91. 11. Bindra K, Berry C, Rogers J et al. Abnormal haemoglobin levels in acute coronary syndromes, QJM. 2010; 99(12): 851-62. 12. Yancy CW, Jessup M, Bozkurt M et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American college of cardiology foundation / American heart association task force on practice guidelines, Journal of the American College of Cardiology. 2013; 62(16): 147-239. 13. Anand IS, Anemia and chronic heart failure. Journal of the American College of Cardiology. 2008; 52(7): 501-511. 14. Mozos I. Mechanisms Linking Red Blood Cell Disorders and Cardiovascular Diseases. BioMed Research International. 2015; Article ID 682054: p1-12. 15. Carson JA, Duff A, Poses RM, Berlin JA, Spence RK, Trout R, et al. Effect of anemia and cardiovascular disease on surgical mortality and morbidity. Lancet 1996;348:1055-60. 16. Rodr
Disclaimer: The Views and opinions expressed in the articles are of the authors and not of the journal.
Editor-In-Chief
Journal Office
Mid City Hospital, 3-A Shadman II
Jail Road, Lahore ,Pakistan
Mid City Hospital, 3-A Shadman II
Jail Road, Lahore ,Pakistan
Managing Editor
Dr. Intan Juliana Abd Hamid
Support & Help
Support & Help
Assistant Editor
Dr. Sadia Shabbir Hussain
Support & Help
Support & Help
Digital Content Editor
Dr. Khalid Masud
Administrator
Administrator