www.apjph.comwww.apjph.com

Ref Number = ASPR0025
When to Test for Food Allergy in Atopic Dermatitis Cases
Raynald Takumansang Department of Child Health, Sam Ratulangi University, Manado, Indonesia E-mail: enal_takumansang@yahoo.com
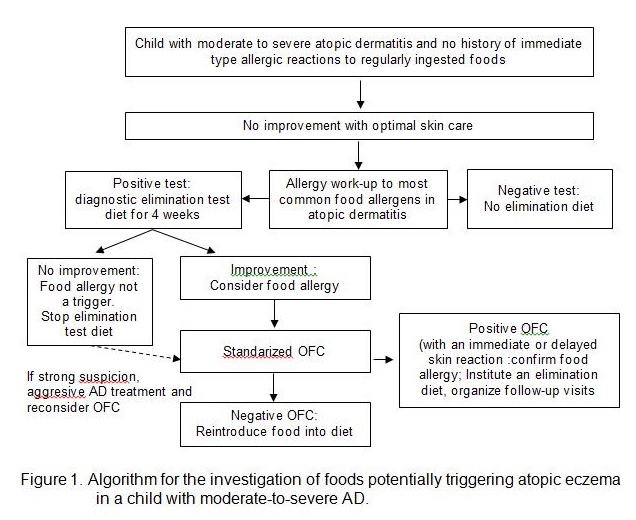
Atopic dermatitis (AD) is a chronic relapsing pruritic in?ammatory disease of the skin frequently associated with allergen sensitization, raised serum immunoglobulin E (IgE) levels, and a family history of allergic diseases. AD affects a large number of children in industrialized countries with an incidence of 10% to almost 30%, according to published data. Its onset is typically in early infancy even though some patients may develop AD later in life. The incidence of AD is estimated to be 1.7% in adolescents, 47.6% of them with first symptoms in early childhood. The reason for persistence of AD into adulthood has not been established, but a genetic predisposition is suspected. Adult-onset AD is rare, occurring in 9% to 14% of cases. Non-AD (not related to IgE-type sensitization) is more common in preschool children or adults with a prevalence of 45% to 64% in children and 40% in adults.10 Children with non-AD have been reported to have a lower risk of developing asthma than atopic children. Several studies have shown that allergens participate actively to cause inflammation after ingestion of specific food in children with AD. Atopic dermatitis is associated with an increase in speci?c IgE (sIgE) to foods, which is often already detectable early in childhood. Food allergy is an important etiology to consider in children with moderate-to-severe atopic dermatitis recalcitrant to typical topical therapy, and responsible in one-third of children with a moderate-to-severe atopic dermatitis. Cow?s milk, hen?s egg, peanut, wheat, soy, nuts, and ?sh are responsible for >90% of food allergy in children with atopic dermatitis. An allergy work-up should be considered in children with a moderate to severe atopic dermatitis despite optimal skin care and currently ingesting a potential suspected food, because this may actively contribute to food-induced atopic dermatitis. Allergy work up is indicated in children with persisting symptoms of atopic dermatitis or allergen related symptoms, particularly in case of other concurrent atopic symptoms. In children less than 3 - 4 years with food allergy usually show symptoms from two or more organ systems concomitantly, but in atopic dermatitis, the children may only show one severe persisting symptom. In children above 4 years with severe persisting atopic dermatitis and without sufficient effect of topical steroids, should be tested for food allergy. Based on practice recommendations, food-triggered AD was defined by positive clinical history of improvement of dermatitis upon food removal or worsening dermatitis upon introduction of causative food and supportive SPT (>3 mm wheal) or specific IgE (>0.35 kU/L) testing (20, 21) to the trigger food. Eczema unrelated to food was defined when either clinical history or laboratory testing were negative. Patients for whom clinical history or laboratory tests were supportive but evidence was lacking in the other category were considered equivocal and not included in further analysis. The diagnosis of food allergy in atopic dermatitis is currently based on the clinical history, skin prick tests, or blood test screening, followed by an elimination diet and/or standardized oral food challenge (OFC), as recomended in the published guidelines for the diagnosis of food hypersensitivity (Figure 1). IgE-mediated immediate reactions can be evaluated by skin prick test and allergen-specific serum IgE tests. These tests alone have low predictive value as it might give false positive reaction. Double-blind-placebo-controlled food challenge (DBPCFC) remain the gold standard in the diagnosis of food allergy. Prevalence of food allergy proven by DBPCFC is 33%-63%. Once an underlying food allergy is con?rmed, the avoidance of the causative food is generally recommended and usually leads to an improvement of the atopic dermatitis. ASPR0025 - 1
Keywords: Food Allergy ; Atopic Dermatitis ; Hypersensitivity ; Immunoglobulin E ; Oral food challenge ; Double-blind-placebo-controlled food challenge
Refference:
Bergmann MM, Caubet JC, Boguniewicz M, Eigenmann PA. Evaluation of Food Allergy in Patients with Atopic Dermatitis. J Allergy Clin Immunol : In Practice 2013;1:22-8. Chang A, Robison R, Cai M, Singh AM. Natural history of food triggered atopic dermatitis and development of immediate reactions in children. J Allergy Clin Immunol Pract. 2016;4(2)229-36. Dhar S, Srinivas SM. Food Allergy in Atopic Dermatitis. Indian J Dermatol 2016;61(6):645-8. Host A, Andrae S, Charkin S, Vazquez C, Dreborg S, et al. Allergy Testing in Children: why, who, when and how?Allergy 2003: 58 : 559-69. Roerdink EM, Blok BM, Blok JL, Schuttelaar MA, Niggemann B, et al. Association of food allergy and atopic dermatitis exacerbations. Ann Allergy Asthma Immunol 2016;116(4):334-8.
Disclaimer: The Views and opinions expressed in the articles are of the authors and not of the journal.
Editor-In-Chief
Journal Office
Mid City Hospital, 3-A Shadman II
Jail Road, Lahore ,Pakistan
Mid City Hospital, 3-A Shadman II
Jail Road, Lahore ,Pakistan
Managing Editor
Dr. Intan Juliana Abd Hamid
Support & Help
Support & Help
Assistant Editor
Dr. Sadia Shabbir Hussain
Support & Help
Support & Help
Digital Content Editor
Dr. Khalid Masud
Administrator
Administrator