www.apjph.comwww.apjph.com

Ref Number = ASPR0043
Persistent Pulmonary Hypertension of Newborn
(Pediatric Cardiology Point of View)
Syarif Rohimi Department of Pediatric Harapan Kita Women and Children Hospital Email: Syarohmi@yahoo.com
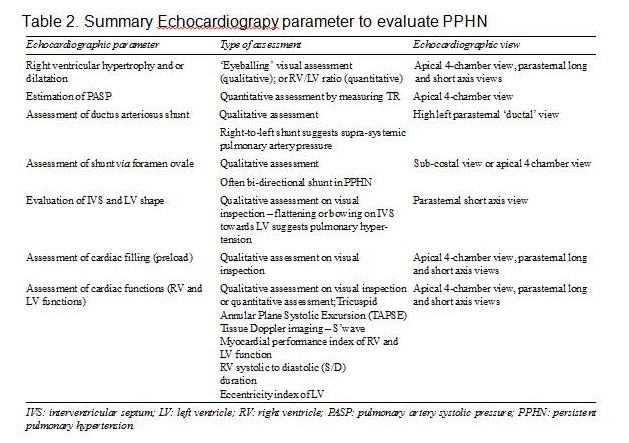
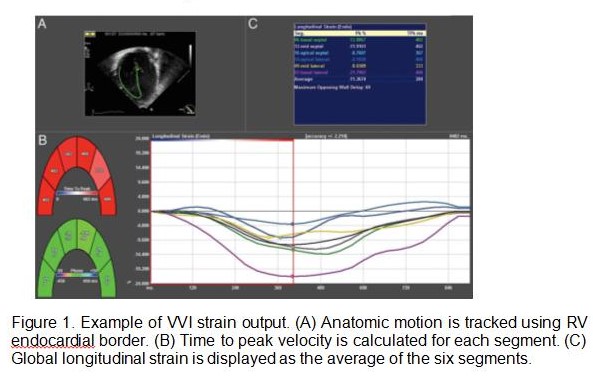
Persistent (PPHN) is a common problem, with an incidence of approximately 1 in 500 live births and mortality of up to 20%. It may be associated with perinatal asphyxia and meconium aspiration with pulmonary parenchymal disease.1 PPHN is often secondary to parenchymal lung disease (meconium aspiration syndrome, pneumonia or respiratory distress syndrome) or lung hypoplasia (with congenital diaphragmatic hernia or oligohydramion) but can also be idiopathic.2 PPHN can also be seen in premature infants and characterized by an abnormal vascular bed that has increased muscularization of vascular smooth muscle cells, distal extension of muscle into non muscularized vessels, arrested vascular growth, increased collagen and elastin deposition in medial arterial layers. PPHN defined a failure of normal postnatal fall in pulmonary vascular resistance leading to impaired oxygenation, Right Ventricle (RV) failure, and pulmonary-to-systemic shunting. Secondary consequences: low cardiac output as left-heart preload compromise, decreased pulmonary venous return and mechanical effects of a pressure/volume- loaded RV on left-heart filling. RV is functioning at higher pressure and volume, which can cause hypertrophy, dilation, and failure. Inadequate ventilation and decreased LV output can lead to respiratory and metabolic acidosis, which in turn causes myocardial dysfunction, worsening pulmonary hypertension, progressive hypoxia, systemic hypoperfusion, and hypotension. This vicious cycle can then worsen to point that cardio-pulmonary or pulmonary bypass with venoarterial or venovenous. Diagnosis of PPHN is based on clinical evidence of labile hypoxemia often associated with differential cyanosis.1,2,3 Echocardiography is the gold standard to confirm diagnosis and to monitor efficacy of specific therapeutic interventions in PPHN.3 The diagnosis is confirmed by echocardiographic demonstration of ? (a) right-to-left or bidirectional shunt at the ductus or foramen ovale and/or, (b) flattening or leftward deviation of the interventricular septum and/or, (c) tricuspid regurgitation, and (d) absence of structural heart disease.2 Comprehensive echocardiographic study should be aimed at excluding structural heart defects associated with pulmonary hypertension (especially total ab- normal pulmonary venous return or left-sided heart problems). For pulmonary hypertension with no structural heart disease, standard follow-up using TNE can be indicated to assess the effect of treatment on PA pressures, RV function, ductal patency, and shunt direction at the ductal and atrial levels. ASPR0043 - 1 The severity of pulmonary hypertension is best assessed by measuring pulmonary artery (PA) pressure. It can also be indirectly assessed by assessing interventricular septum and LV shape. ASPR0043 - 2 The shunt across PDA may be bidirectional or purely right to left depending upon PA pressure in relation to systemic pressure. The shunt across foramen ovale is often bidirectional. RV cardiac output may be decreased in presence of high PVR and RV dysfunction, and LV cardiac output may be decreased from decreased LV preload (decreased pulmonary venous return) and LV dysfunction (37). A thorough assessment of adverse adaptation in persistent pulmonary hypertension may include: - Recognition of RV hypertrophy with or without RV dilatation - Estimation of pulmonary artery pressure - Assessment of shunt across ductus arteriosus and foramen ?ovale - Assessment of interventricular septum and LV shape - Evaluation of RV and LV function - Cardiac filling (preload assessment) - Measurement of RV and LV cardiac output.6 ,7 Once the diagnosis of PPHN is confirmed by echocardiography, the clinical course and the effects of medical interventions can be monitored using NPE with the emphasis on: 1. pulmonary artery pressure and PVR,?2. Myocardial performance, and?3. shunting through ductus arteriosus and open foramen ovale. Tissue Doppler Imaging (TDI) is a relatively new ultrasound modality derives measurement of contraction and relaxation velocities directly from myocardium. This offers a quantitative assessment of both systolic and diastolic function by assessing displacement of mitral and tricuspid annuli during cardiac cycle. Longitudinal myocardial motion velocity (base to apex in systole and the reverse in diastole can be measured from the mitral and tricuspid valve annuli..2,5 ASPR0043 - 3 Lung volume recruitment with optimal use of positive end-expiratory pressure or mean airway pressure and/or surfactant is very important in secondary PPHN due to parenchymal lung disease. Other management strategies include optimal oxygenation, avoiding respiratory and metabolic acidosis, blood pressure stabilization, sedation, and pulmonary vasodilator therapy. Failure of these measures leads to consideration of extracorporeal membrane oxygenation, although this rescue therapy is needed less frequently with advances in medical management.3 TAPSE ,4 mm, Global Longitudinal Strain (GLS) greater than or equal to 29%, and a predominantly right-to-left PDA shunt is associated with poor outcomes in infants with PPHN.4 ASPR0043 - 4
Keywords: PPHN, RV indices, Echocardiography, TDI, GLS


Refference:
1. Sharma V. Berkelhamer S, Lakshiminrusimha S. Persistent Pulmonary Hypertension of the newborn. Maternal Health, Neonatology, and Perinatology,2015;15: 2. Writing group of the American Society of Echocardiography (ASE) in collaboration with the European Association of Echocardiography (EAE) and the Association for European Pediatric Cardiologists (AEPC). Targeted Neonatal Echocardiography in the Neonatal Intensive Care Unit: Practice Guidelines and Recommendations for Training. J Am Soc Echocardiogr 2011;24:1057-78 3. Khuffash A El, McNamara P Targeted Neonatal Echocardiography. Teaching Manual, second Ed. 2014. 1-55.Persistent Pulmonary Hypertension of the newborn. Lakshiminrusimha S, Keszler M. NeoReviews 2015; 12: 4. Malowitzn JR, Forsha DE, Smith B, Michael CM, Barker PC, Tatum GH. Right ventricular echocardiographic indices predict poor outcomes in infants with persistent pulmonary hypertension of newborn. EHJ 2015;16,1224-31 5. Boode WP, Singh Y, Molnar Z3, Schubert U, Savoia M, Sehgal A, Philip T. Levy PT, McNamara PJ, and El-Khuffash AE. Application of Neonatologist Performed Echocardiography in the assessment and management of persistent pulmonary hypertension of the newborn. Pediatric Research 2018; 84:S68?S77. 6. Moss S, Kitchiner DJ, Yoxall CW, Subhedar NV. Evaluation of echocardiography on the neonatal unit. Arch Dis Child 2003;88:F287?F91. 7. Singh Y, Tisso C .Echocardiographic Evaluation of Transitional Circulation for the Neonatologists. Frontiers in Pediatrics, 2018: 140:
Disclaimer: The Views and opinions expressed in the articles are of the authors and not of the journal.
Editor-In-Chief
Journal Office
Mid City Hospital, 3-A Shadman II
Jail Road, Lahore ,Pakistan
Mid City Hospital, 3-A Shadman II
Jail Road, Lahore ,Pakistan
Managing Editor
Dr. Intan Juliana Abd Hamid
Support & Help
Support & Help
Assistant Editor
Dr. Sadia Shabbir Hussain
Support & Help
Support & Help
Digital Content Editor
Dr. Khalid Masud
Administrator
Administrator