www.apjph.comwww.apjph.com

Volume 1, July-Sept 2018
Annotation:

What can Pediatricians do to address child health in South and Southeast Asia?
Zulfiqar A Bhutta
Zulfiqar A Bhutta
Author’s Affiliation:
Founding Director - Centre of Excellence in Women & Child Health - The Aga Khan University, South Central Asia, East Africa & United Kingdom - Karachi 74800, Pakistan
Robert Harding Chair in Global Child Health & Policy - Co-Director, SickKids Centre for Global Child Health - The Hospital for Sick Children - Toronto ON,M5G A04, Canada
President - International Pediatric Association
Founding Director - Centre of Excellence in Women & Child Health - The Aga Khan University, South Central Asia, East Africa & United Kingdom - Karachi 74800, Pakistan
Robert Harding Chair in Global Child Health & Policy - Co-Director, SickKids Centre for Global Child Health - The Hospital for Sick Children - Toronto ON,M5G A04, Canada
President - International Pediatric Association
Received on: 26-Aug-2018
Accepted for Publication: 23-Aug-2018
Article No: 188266f4095557
PDF - Full Text
Despite the remarkable reduction in under 5 child mortality globally in the wake of the Millennium Development Goals (MDGs), a little under 6 million children still perish every year before reaching their fifth birthday. A large proportion, almost 46% die within the neonatal period (the first 28 days of life), many during the process of birth or within the first 24 hours thereafter, the majority within the neonatal period (1).
South Asia, mainly comprising the countries who are signatories to the South Asia Association for Regional Cooperation (SAARC), namely India, Pakistan, Bangladesh, Nepal, Bhutan, Maldives, Sri Lanka and Afghanistan. The combined population of SAARC countries is around 1.67 billion, representing approximately 23.5% of the total world’s population. With the inclusion of Afghanistan, the region now houses countries with the highest child mortality rates in Asia. Of the eight SAARC countries, Afghanistan has the highest under-5 mortality rates (97) and Sri Lanka and the Maldives have the lowest under-5 mortality rate (10). Some 22% of maternal deaths globally and almost 31% of all child deaths are in South Asia, with 57% of all child deaths occurring in the neonatal period (2). While there has been progress in the period between 2000 and 2015, this has been uneven. Sri Lanka was always leagues ahead of its neighbors in progress and investments in primary care and in contrast, while Bangladesh and Nepal had huge challenges when reviewed over a decade ago (3), both were able to achieve the MDG targets for maternal and child survival. In the year 2000, the MDG4 target was set with specific targets for mortality re-induction by two- thirds by the year 2015. A recent countdown review indicates that out of the SAARC countries surveyed, except for India, Pakistan and Afghanistan, all the other SAARC countries have already achieved the MDG 4 goals.
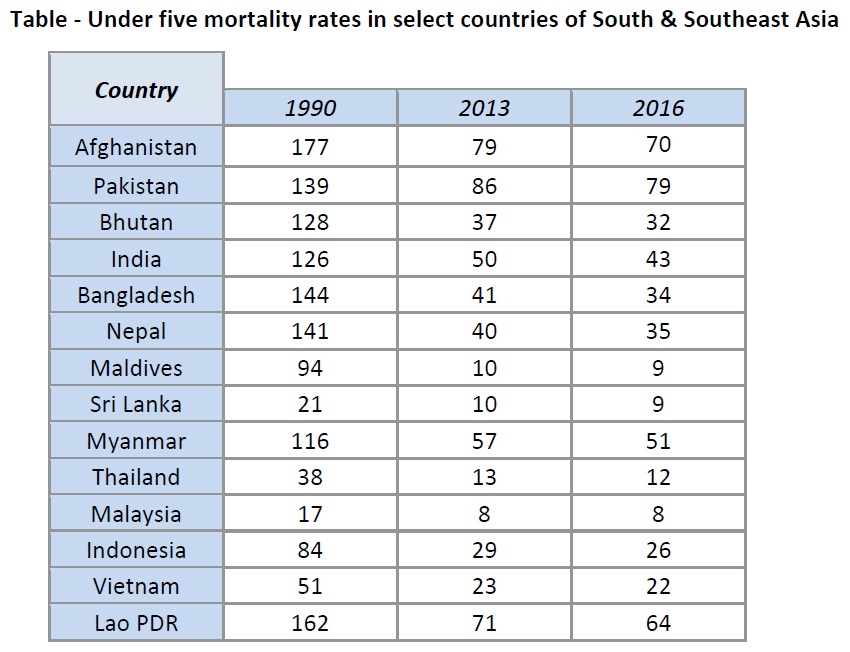
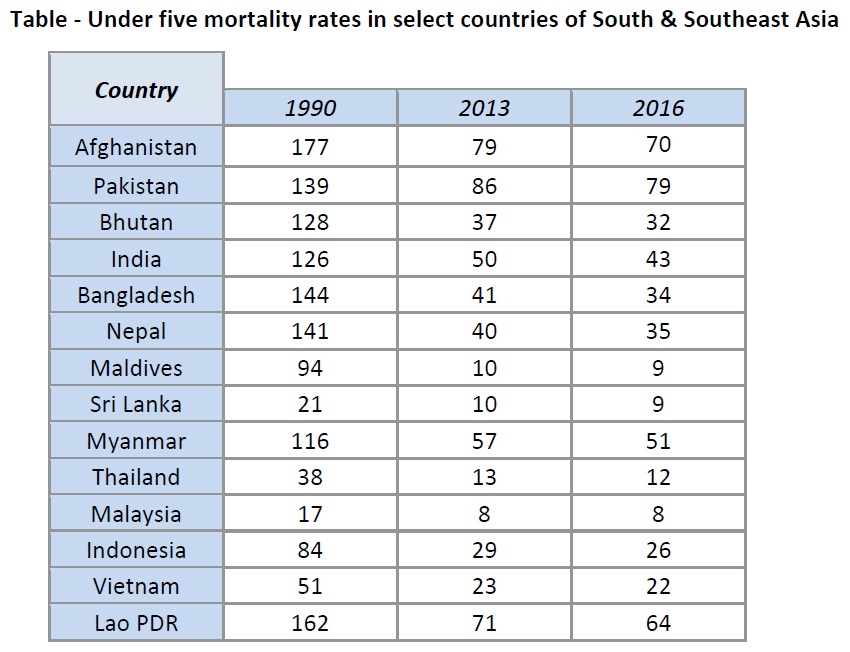
In contrast many countries in Southeast Asia region seems to have made much progress over time. When last reviewed a decade ago (4), we identified three major patterns of maternal and child mortality reduction: early, rapid downward trends (Brunei, Singapore, Malaysia, and Thailand); initially high declines (sustained by Vietnam but faltering in the Philippines and Indonesia); and high initial rates with a downward trend (Laos, Cambodia, and Myanmar). Since then the region has largely met the MDG targets except for Lao PDR and the human displacement emergency in Myanmar. Table 1 summarizes some of the trends in mortality over time in South and Southeast Asia (5)
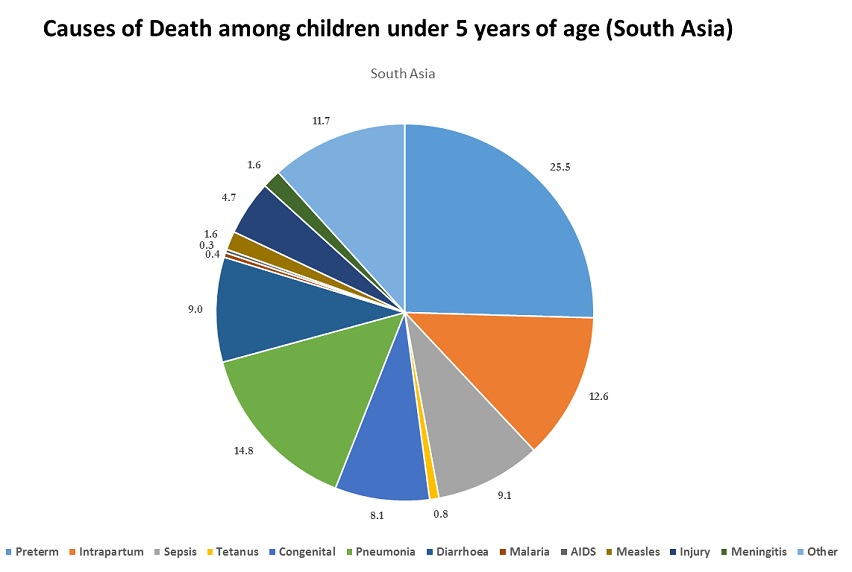
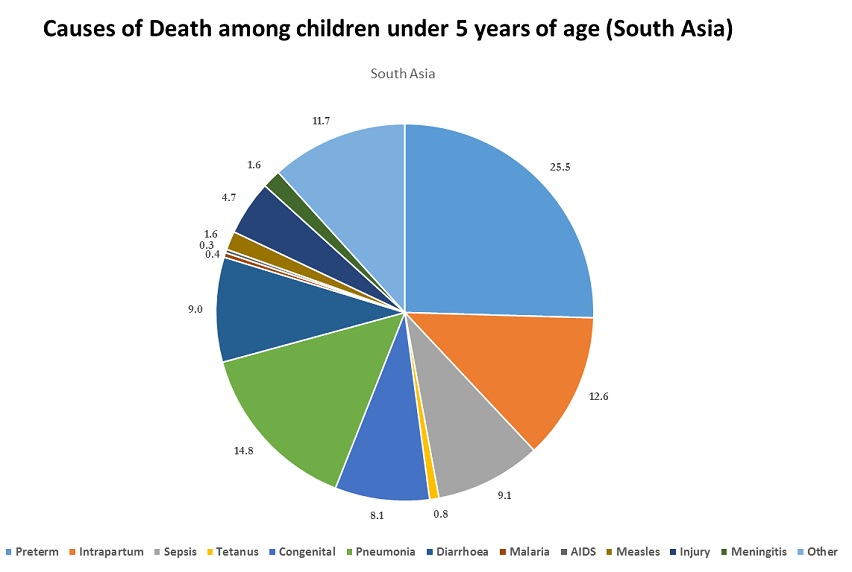
The causes of newborn and child mortality in the region are well known and summarized in Figure 1. For many of these issues the specific evidence-based interventions are well known and need scaling up and targeting marginalized and poor populations. For averting preventable neonatal mortality (6), major interventions need to target mothers and care during pregnancy and childbirth. These include appropriate care of the mother in pregnancy, use of antenatal steroids in preterm labor, antibiotics for preterm premature rupture of membranes, appropriate care during birth and in the first 48 hours after birth. Perinatal asphyxia can account for up to half of all newborn deaths in the first week of life and can be associated with significant neonatal morbidity and developmental disability. Many cases of perinatal asphyxia are difficult to predict and hence appropriate facilities for recognition and neonatal resuscitation must be available in all birthing facilities, and staff trained therein. At the very basic level, encouraging facility-based births in the hands of skilled-birth attendants with appropriate basic equipment is a key intervention. The development of Helping Babies Breathe training modules by the American Academy of Pediatrics is a key step in the direction of global scale-up of such strategies (7).
While it may be difficult to prevent prematurity entirely, cost-effective strategies for care at birth and prevention of hypothermia are possible. These require attention to the prevention of hypothermia, institution of Kangaroo Mother Care (KMC) in appropriate facility settings and possible community use. To address other complications of prematurity, appropriate care of sick and small babies is needed. There is a great need for scaling up appropriate respiratory care strategies in referral facilities such as the use of low cost continuous positive airway pressure (CPAP) and monitoring systems. Although, there have been remarkable reductions in neonatal tetanus, neonatal sepsis remains a major cause of morbidity and mortality in newborn and although vertical transmission is possible, the majority of these infections are community-acquired and hence, potentially preventable. The common bacterial and viral pathogens causing neonatal sepsis are well recognized from recent community-based research in South Asia (8). Hand hygiene, and the use of birth kits, followed by appropriate cord care are important interventions to prevent infection. Emerging evidence from various SAARC countries indicates that the use of cord chlorhexidine may be associated with significant reduction in the risk of neonatal omphalitis and sepsis. Given the high rates of infections in community settings and potential delays in recognition and referral, there is increasing attention to community-based detection and management of potential neonatal infections and other problems, and several studies have demonstrated the benefit of such an approach (9, 10).
The development of vaccination strategies for childhood diarrhea and pneumonia such as Hib, pneumococcal and Rotavirus vaccines, offers a huge opportunity for addressing major post-neonatal child deaths (11). However, scaling up immunization coverage also requires behavior change at the level of parents and families in addition to service delivery by health care professionals and the health system. To illustrate, childhood immunization requires parental awareness and partaking of vaccinations as part of the expanded programs of immunization. Issues of vaccine hesitancy and misinformation lie behind the reluctance of many families to seek these preventive interventions in a timely manner (12). Similarly maternal education is a key element in promotion of healthy practices, nurturing care and appropriate infant and young child feeding practices (13). In many countries of the region, early initiation of and exclusive breast-feeding rates remain suboptimal. In South Asia a major contributor to poor progress is the poor status of safe water and sanitation facilities. Between 20% and 30% of the population still does not have access to safe water and over a third of the rural population practices open defecation. This must change for us to see an end to preventable diarrhea and pneumonia deaths. The contribution of air pollution to the burden of child deaths has been quantified in Africa (14) and needs to receive appropriate attention in South and Southeast Asia.
To make lasting progress all Pediatricians must become closely engaged in addressing the social determinants of health and the interlinked opportunities that the SDGs offer in this regards. Maternal and child undernutrition is an important determinant of child mortality and long-term adverse outcomes including development. In addition to poverty and misdistribution of resources, the status of women in society, empowerment, ethnicity and race play a critical role in existing inequities in care and access. Gender inequities and high fertility rates are a major rate limiting factor in Asia. Most people living in rural areas and urban slums live in abysmal conditions and have limited access to quality healthcare services. Appropriate targeting, poverty alleviation strategies such as conditional cash transfers, employment schemes and good governance are essential elements in provoking change. This also means addressing the plight of children and families living in conflict zones and displaced populations.
National, regional and global Pediatric Associations have a huge responsibility for highlighting these issues systematically and creating the groundswell of support for action. They can be the watchdogs for ensuring that governments and public health officials fulfill their responsibility for guaranteed primary care and preventive strategies for all. Some forty years after the Alma Ata declaration (14), this is what all Pediatricians and health-care professionals must stand behind.

References
- Liu L, Oza S, Hogan D, Chu Y, Perin J, Zhu J, Lawn JE, Cousens S, Mathers C, Black RE. Global, regional, and national causes of under-5 mortality in 2000-15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet. 2016;388:3027-3035.
- Akseer N, Kamali M, Arifeen SE, Malik A, Bhatti Z, Thacker N, Maksey M, D'Silva H, da Silva IC, Bhutta ZA. Progress in maternal and child health: how has South Asia fared? BMJ. 2017;357:j1608. doi: 10.1136/bmj.j1608.
- Bhutta ZA, Gupta I, de'Silva H, Manandhar D, Awasthi S, Hossain SM, Salam MA. Maternal and child health: is South Asia ready for change? BMJ. 2004;328:816-9
- Acuin CS, Khor GL, Liabsuetrakul T, Achadi EL, Htay TT, Firestone R, Bhutta ZA. Maternal, neonatal, and child health in southeast Asia: towards greater regional collaboration. Lancet. 2011;377:516-25
- UN Interagency Group for Child Mortality Estimation. Levels and Trends of Child Mortality 2017.
- Bhutta ZA, Das JK, Bahl R, Lawn JE, Salam RA, Paul VK, Sankar MJ, Blencowe H, Rizvi A, Chou VB, Walker N; Lancet Newborn Interventions Review Group; Lancet Every Newborn Study Group. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet. 2014;384:347-70.
- Dol J, Campbell-Yeo M, Murphy GT, Aston M, McMillan D, Richardson B. The impact of the Helping Babies Survive program on neonatal outcomes and health provider skills: a systematic review. JBI Database System Rev Implement Rep. 2018;16:701-737.
- Saha SK, Schrag SJ, El Arifeen S, Mullany LC, Shahidul Islam M, Shang N, Qazi SA, Zaidi AKM, Bhutta ZA, Bose A, Panigrahi P, Soofi SB, Connor NE, Mitra DK, Isaac R, Winchell JM, Arvay ML, Islam M, Shafiq Y, Nisar I, Baloch B, Kabir F, Ali M, Diaz MH, Satpathy R, Nanda P, Padhi BK, Parida S, Hotwani A, Hasanuzzaman M, Ahmed S, Belal Hossain M, Ariff S, Ahmed I, Ibne Moin SM, Mahmud A, Waller JL, Rafiqullah I, Quaiyum MA, Begum N, Balaji V, Halen J, Nawshad Uddin Ahmed ASM, Weber MW, Hamer DH, Hibberd PL, Sadeq-Ur Rahman Q, Mogan VR, Hossain T, McGee L, Anandan S, Liu A, Panigrahi K, Abraham AM, Baqui AH. Causes and incidence of community-acquired serious infections among young children in south Asia (ANISA): an observational cohort study. Lancet. 2018;392:145-159.
- Baqui AH, Saha SK, Ahmed AS, Shahidullah M, Quasem I, Roth DE, Samsuzzaman AK, Ahmed W, Tabib SM, Mitra DK, Begum N, Islam M, Mahmud A, Rahman MH, Moin MI, Mullany LC, Cousens S, El Arifeen S, Wall S, Brandes N, Santosham M, Black RE; Projahnmo Study Group in Bangladesh. Safety and efficacy of alternative antibiotic regimens compared with 7 day injectable procaine benzylpenicillin and gentamicin for outpatient treatment of neonates and young infants with clinical signs of severe infection when referral is not possible: a randomised, open-label, equivalence trial. Lancet Glob Health. 2015 May;3(5):e279-87. doi:10.1016/S2214-109X(14)70347-X.
- Mir F, Nisar I, Tikmani SS, Baloch B, Shakoor S, Jehan F, Ahmed I, Cousens S, Zaidi AK. Simplified antibiotic regimens for treatment of clinical severe infection in the outpatient setting when referral is not possible for young infants in Pakistan (Simplified Antibiotic Therapy Trial [SATT]): a randomised, open-label, equivalence trial. Lancet Glob Health. 2017 Feb;5(2):e177-e185. doi: 10.1016/S2214-109X(16)30335-7
- Bhutta ZA, Das JK, Walker N, Rizvi A, Campbell H, Rudan I, Black RE; Lancet Diarrhoea and Pneumonia Interventions Study Group. Interventions to address deaths from childhood pneumonia and diarrhoea equitably: what works and at what cost? Lancet. 2013 Apr 20;381(9875):1417-1429. doi:10.1016/S0140-6736(13)60648-0.
- Mohanty S, Carroll-Scott A, Wheeler M, Davis-Hayes C, Turchi R, Feemster K, Yudell M, Buttenheim AM. Vaccine Hesitancy in Pediatric Primary Care Practices. Qual Health Res. 2018 Jun 1:1049732318782164. doi: 10.1177/1049732318782164.
- Britto PR, Lye SJ, Proulx K, Yousafzai AK, Matthews SG, Vaivada T, Perez-Escamilla R, Rao N, Ip P, Fernald LCH, MacMillan H, Hanson M, Wachs TD, Yao H, Yoshikawa H, Cerezo A, Leckman JF, Bhutta ZA; Early Childhood Development Interventions Review Group, for the Lancet Early Childhood Development Series Steering Committee. Nurturing care: promoting early childhood development. Lancet. 2017;389:91-102.
- Bhutta ZA, Ali S, Cousens S, Ali TM, Haider BA, Rizvi A, Okong P, Bhutta SZ, Black RE. Alma-Ata: Rebirth and Revision 6 Interventions to address maternal, newborn, and child survival: what difference can integrated primary health care strategies make? Lancet. 2008;372:972-89
Disclaimer: The Views and opinions expressed in the articles are of the authors and not of the journal.
Editor-In-Chief
Journal Office
Mid City Hospital, 3-A Shadman II
Jail Road, Lahore ,Pakistan
Mid City Hospital, 3-A Shadman II
Jail Road, Lahore ,Pakistan
Managing Editor
Dr. Intan Juliana Abd Hamid
Support & Help
Support & Help
Assistant Editor
Dr. Sadia Shabbir Hussain
Support & Help
Support & Help
Digital Content Editor
Dr. Khalid Masud
Administrator
Administrator